Melanotan 1 is a synthetic analogue of alpha-melanotocyte stimulating hormone. It is used clinically, in Europe, to prevent sun-related skin damage (i.e. phototoxicity) from occurring in people suffering from erythropoietic protoporphyria. Though initially developed as a sunless tanning agent, melanotan 1 has been found to have a number of physiologic effects on blood pressure, feeding behavior, central nervous system function, and more. The peptide is in phase 3 clinical trials for the treatment of polymorphose light eruption and is in phase 2 clinical trials for the treatment of actinic keratosis (a specific type of skin damage caused by the sun) and its more serious counterpart, squamous cell carcinoma.
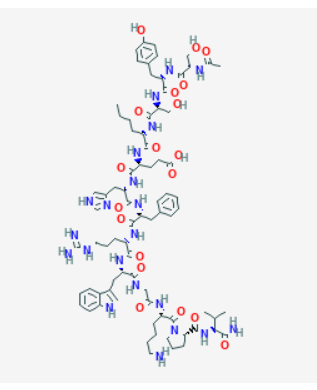
Sequence: Ser-Tyr-Ser-Nle-Glu-His-D-Phe-Arg-Trp-Gly-Lys-Pro-Val
Molecular Formula: C78H111N21O19
Molecular Weight: 1646.874 g/mol
PubChem CID: 16154396
CAS Number: 75921-69-6
Synonyms: Afamelanotide, Scenesse, CUV1657, MT-1
Melanotan 1 is very similar to naturally occurring alpha melanocyte stimulating hormone (alpha-MSH). Alpha-MSH is primarily known for its influence on melanocytes, the cells in skin and hair responsible for pigmentation. This function is mediated via strong binding to melanocortin receptor 1. Alpha-MSH is a non-selective full agonist of melanocortin receptors 1, 3, 4, and 5.
Melanotan 1 differs from alpha-MSH by a single amino acid and was actually first developed as a sunless tanning agent. Research into melanocortin receptors and their effects was relatively limited at the time and scientists quickly discovered that while melanotan 1 did indeed cause pigmentation, it also increase sexual arousal, boosted appetite, and altered baseline metabolism. Subsequent study of melanotan 1 and other melanocortin-binding proteins helped scientists to better understand the melanocortin signaling system.
MT-1 has been studied in phase 1 clinical trials for its effect on tanning in humans exposed to ultraviolet radiation. The research showed that subjects administered MT-1 were 75% more likely to tan and 47% less likely to experience sunburn. Compared to controls, subjects given melanotan 1 required 50% less exposure to ultraviolet light to achieve equivalent tanning. They also retained their tan for three weeks longer than those exposed only to UV light[1]. There is some thought among scientists that melanotan 1 could be used to boost tanning in high UV settings to protect against sunburn and the long-term effects of ultraviolet skin damage. This could be particularly useful in individuals with poor-tanning skin types (referred to as type I and type II by the Fitzpatrick scale).
Research in individuals with variant MC1 receptors shows that they are less likely to tan than the average individual. As it turns out, administration of melanotan 1 in this setting increases melanin density and tanning substantially, helping to protect people who do not tan well and are most in need of photoprotection[2]. These are individuals who get limited benefit from sunscreen and, in order to prevent skin cancer, must limit their sun exposure a great deal. This research could open pathways to better UV protection and reduce rates of skin cancer substantially.
There is also interest in using melanotan 1 to treat vitiligo. A small phase 1 trial showed that using melanotan 1 in conjunction with UVB light therapy stimulated both melanin production and the proliferation of the melanocytes that produce melanin. Nearly half of treated patients showed improved pigmentation of vitiligo lesions and a faster rate of repigmentation[3]. Research shows that combining melanotan 1 treatment with existing treatment modalities of vitiligo produces synergistic effects and improved aesthetic outcomes in shorter periods of time[4]. If successful in vitiligo treatment, there may be applications for melanotan 1 treatment in the setting of hypopigmented scars, etc.
Actinic keratosis, also called solar keratosis, is a crusty scaly growth of skin caused by overexposure to UV light. It is considered a precancerous lesion that will eventually lead to squamous cell carcinoma (one type of skin cancer) if left untreated. There are more than 400,000 cases every year. Though obvious lesions can be removed by a dermatologist or surgeon, the vast majority are so small that they cannot be seen or even felt. Melanotan 1 is being investigated as a possible first-line agent for treating these invisible lesions and for preventing their progression to full-blown skin cancer.
Research in hypertensive (high blood pressure) mice has revealed that melanotan 1 can protect against high blood pressure without affecting animals that have normal blood pressure[5]. This is important because current blood pressure medications can cause hypotension, which can lead to loss of consciousness, stroke, heart attack, and more. This side effect of blood pressure medications is more common in the elderly, thanks in part to their labile physiology. The ability to regulate high blood pressure without causing significant lows makes melanotan 1 the perfect candidate for exploring further drug development.
Research in transgenic mice indicates that melanotan 1 may protect the brain against the kind of damage that leads to cognitive decline and Alzheimer’s disease. The study, which used a mouse model of moderate Alzheimer’s disease (AD), indicated that melanotan 1, even in minuscule doses, reduces the level of amyloid beta plaques in the brain, protects neurons from death, and improves clinical measures of cognitive function as well as laboratory measures of synaptic transmission. In the same study, blocking the effects of melanotan 1 at the MC4 receptor prevented all of the peptide’s favorable effects[6].
The benefit of melanotan 1 action at the MC4 receptor has been explored in other studies as well. Research, also in mice, shows that MC4 receptor stimulation can boost neurogenesis and lead to cognitive recovery in AD. It is one of the few studies to show improvement in the condition rather than simply slowing decline[7]. Once daily administration of MT-1 reduces levels of all AD-related biomarkers, indicating that the peptide actually works through multiple pathophysiological pathways[8].
The MC4 receptor is the only melanocortin receptor known to be expressed on astrocytes, the cells that protect neurons and provide them with nutrition. Research in rats indicates that melanotan 1 improves astrocyte functioning by increasing levels of brain-derived neurotrophic factor (BDNF)[9]. BDNF is critical to protecting synapse stability and neurogenesis in general.
It isn’t just biomarkers in AD that improve following MT-1 treatment. Research in gerbil models of a stroke lasting ten full minutes reveals that treatment with nanomolar doses of melanotan 2 can reduce brain damage, including neuron death, and improve recovering of learning and memory. What is really exciting is that these effects are achieved even melanotan 1 is administered 9 hours after a stroke[10]. It is thought that MT-1 activates repair mechanisms that improve synaptic plasticity and promote long-lasting functional recovery by allowing the brain to reroute learning and memory to healthier areas. The lynch pin in this process appears to be expression of the Zif268 gene. Zif268 is over-expressed in animals given melanotan-1. The same gene is also over-expressed in the models of Alzheimer’s disease showing cognitive improvement.
Research in rats undergoing heart attack has shown that melanotan 1 and other melanocortins can help to reduce injury and improve circulatory parameters. Administration of MT-1 during CPR and in conjunction with epinephrine helps to restore baseline arterial pressure and heart rate, reverses metabolic acidosis, reduces inflammatory markers, and improves the expression of genes associated with cardiac function. Overall, the therapy improved survival rate by 81%, a substantial increase that may make melanotan 1 or a similar melanocortin a mainstay of emergency advanced cardiac life support[11].
Research on melanotan 1 has revealed that the MC1 receptor is responsible for pigmentation in skin and hair. For a long time it was thought that this was the receptor’s only function. Recent research in mice, however, has indicated that this receptor plays a role in mediating inflammation in the central nervous system. In multiple sclerosis, for instance, helper T cells cause loss of myelin on neurons, which in turn causes neuron dysfunction and even death. In mice, administration of melanotan 1 interferes with this process and prevents loss of meylin, thus preventing neuron damage. In fact, administration of MT-1 to these mice improved myelin recovery and helped to reestablish neuron signaling[12].
Similar effects as above are also seen in mouse models of uveitis, an inflammatory disorder of the eye that can cause pain and vision loss. Current treatments have a range of side effects, so scientists are constantly searching for alternatives to steroids and immunosuppressive drugs. Alpha-MSH acts to suppress T-cell function, a property mediated through the MC4 receptor and thus mimicked by MT-1[13]. Surprisingly, local administration of MC4 receptor agonists directly to the eye is as effective as systemic administration. This route of administration helps to eliminate systemic side effects.
Melanotan 1 works on several melanocortin receptors, including the MC5 receptor. Stimulation of MC5R promotes the oxidation of fatty acids by muscle and shifts fat cells from fat storage to fat burning[14], [15]. These findings in mice also reveal that the fat burning caused by melanocortin stimulation is complex and involves several receptors and physiologic pathways. That said, melanotan 1 is useful to scientists wishing to explore how fatty acid metabolism can be altered and offers the tantalizing ability to boost baseline physiology without the need for exercise, which could be of tremendous benefit in individuals who are unable to exercise due to